South Africa's ICU crisis: An urgent call to action for beds and skilled medical staff
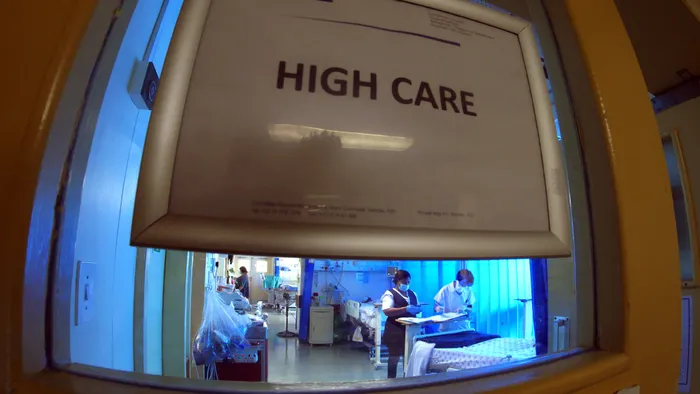
South Africa is facing a critical shortage of ICU beds and skilled staff to man those units
Image: Ian Landsberg/ANA Archive
SOUTH Africa's dire need for ICU beds has become a critical situation and continues to place further strain on the country's already fragile public health system.
Currently, the country is only able to provide a mere five ICU beds per 100,000 people at best, with some provinces seeing numbers drop drastically to as few as one bed per 100,000.
Another area of concern is the constantly diminishing number of skilled medical people who specialise in ICU work.
This stark reality was laid bare by Professor Fathima Paruk, head of the Department of Critical Care Services and Emergency Medicine at the University of Pretoria’s (UP) Faculty of Health Sciences, during her inaugural address entitled “Carpe Diem: Achieving efficient and fair allocation of critical care across South Africa”.
Professor Paruk underscored the gravity of the situation, explaining that the number of ICU beds needed is only expected to grow as patients live longer and face increasing co-morbidities. “Hospitals are going to need more and more ICU beds because patients are living longer. ICU can save lives, and when patients live longer, they have more co-morbidities, so they end up getting sick more often,” she said, highlighting how medical advancements coupled with a shift towards outpatient and home care will likely lead to a parallel surge in demand for high-level critical care.
However, the reality in South Africa’s health system is multifaceted and complex. In the private sector, the adaptability of hospitals means that new ICU beds can be created as needed, yet the public sector remains constrained by existing infrastructure.
“In the public sector, you have X number of beds and that’s it,” explained Paruk. This limitation is exacerbated by geographic disparities across provinces, with access to critical care significantly better in urban centres like Cape Town compared to rural areas such as Limpopo.
Moreover, the struggle for adequate critical care was not just about bed availability. Professor Paruk pointed out a critical shortage of qualified nurses and doctors essential for operating ICU units.
“We are extremely short on them in both the public and private sectors. Only 25% of our ICU nurses are trained in critical care,” she stated.
During her address, Paruk also reflected on the transformative impact of the COVID-19 pandemic on healthcare delivery in the country. While the pandemic brought unprecedented challenges, it also paved the way for innovative solutions. In a notable example, she described how the UP collaborated with Charité University in Berlin, utilising telemedicine to support the Steve Biko Academic Hospital.
The use of a robot named Stevie facilitated remote consultation, showcasing how technology can bridge gaps in critical care. “With telemedicine, you can help stabilise patients, and you can even help with a procedure. We can ultimately enhance the level of care to our community,” she elaborated.
Looking to the future, Professor Paruk is actively involved in a new national ICU audit spearheaded by the Critical Care Society of Southern Africa.
The last such audit was conducted 15 years ago, and Paruk emphasised the importance of updating the data to reflect how the healthcare landscape has changed, especially after the COVID-19 pandemic.
The upcoming audit aims to gather essential statistics from both public and private hospitals regarding the available ICU resources, including bed counts, staffing levels, and equipment availability.
The overarching goal of this initiative is to inform strategic planning and bolster the integrity of South Africa's health system as the country progresses towards implementing the National Health Insurance. Furthermore, the audit seeks to develop a living dashboard for real-time monitoring of ICU capacity, a crucial tool for ensuring patient care continuity amid escalating demands.
DAILY NEWS